
MIGRAINE
Dalam tahun 2002/2004, aku kerap diserang sakit kepala. Kadang kala aku tidak dapat menumpukan
perhatian kepada tugas atau kerja harianku, khususnya di pejabat. Kesakitannya rasa berdenyut-denyut seolah olah seperti kesan cucukan atau ketukan di atas kepala. Aku akan meramas-ramas rambutku atau menepuk-nepuk kepala bagi mengurangkan konsentrasi kesakitan itu. Beberapa kali aku menemui doktor di Pusat Perubatan ATM (PPAT) di MINDEF untuk mendapatkan rawatan. Namun tiada rawatan lanjut, aku hanya
diberikan pain killer untuk mengurangkan kesakitan.
Pada tahun 2004, bila membaca kesah pelbagai penyakit
berkaitan barah termasuk barah otak, ketumbuhan dalam otak (brain tumor) dan
sebagainya, aku mula merasa lebih risau. Apabila mendapati kesakitan yang aku alami tidak berkurangan, aku memohon untuk membuat MRI (scan). MRI ialah Magnetic Resonance Imaging.
Pihak RSAT telah membuat temujanji dengan Hospital ATM di Pangkalan TLDM LUMUT untuk
membuat MRI scan. Bagaimanapun, setelah
menerima laporan, di dapati tiada tanda atau symptom penyakit barah atau tumor. Melalui interview dengan doktor di RSAT
selepas menerima laporan itu, antara soalannya ialah berkaitan pekerjaan, dan
permakanan. Setelah menerangkan makanan
dan minuman kegemaranku, maka doktor mensyaki dan membuat diagnosis bahawa aku
berkemungkinan menghidapi migraine!
Puncanya (suspek) ialah kegemaran ku yang terlampau minum
NESCAFE.
Bayangkan, pada masa itu NESCAFE adalah minuman kegemaranku selama bertahun-tahun. Biasanya aku tidak bersarapan di rumah. Tetapi bila sampai di pejabat, aku akan terus ke pantry untuk membuat secawan nescafe. Dalam pukul 1000H aku akan membuat secawan lagi. Nanti selepas lunch, aku akan membuat secawan lagi.
Bayangkan, pada masa itu NESCAFE adalah minuman kegemaranku selama bertahun-tahun. Biasanya aku tidak bersarapan di rumah. Tetapi bila sampai di pejabat, aku akan terus ke pantry untuk membuat secawan nescafe. Dalam pukul 1000H aku akan membuat secawan lagi. Nanti selepas lunch, aku akan membuat secawan lagi.

Sebelah petang, dalam pukul 2.30 pm atau 3 pm aku akan membuat secawan lagi. Bila balik rumah selepas Asar (minum petang) aku akan membuat secawan Nescafe. Nanti selepas makan malam secawan lagi. Malam-malam ketika buat kerja, mesti ada secawan nescafe di depanku. Maknanya setiap hari, jumlah nescafe yang aku minum ialah TUJUH cawan.
Selepas mendapat maklumat itu, aku pun stop minum nescafe dan tukar kepada
Kopi O. Brand kegemaranku adalah Kopi
Hang Tuah. Original coffee. Tapi beberapa tahun sahaja aku mengambil kopi O,
aku mengalami masalah batuk-batuk. Lalu aku berhenti minum kopi O.

Kini aku menjadikan The Tarik brand ini sebagai menu
harianku, disamping minum susu kambing.

"Migraine merupakan sakit kepala yang berulang-ulang
disebabkan oleh sesuatu sebab. Trigger factor (faktor penyebab) migraine
berkemungkinan faktor hormon seperti ketika datang haid, mengamalkan pil
perancang, faktor persekitaran seperti suhu yang terlalu panas atau sejuk,
cahaya terlalu terang atau bunyi yang terlalu bising, faktor stress seperti
kurang tidur, tension, banyak memikir dll., faktor pemakanan seperti makanan
masam (jeruk, buahan sitrus), makanan berperisa/perasa/pengawet/ pewarna tiruan
(ajinomoto, maggi mee), makanan mempunyai xanthine (cokelat), makanan tenusu
(keju, susu), minuman berkafein (kopi, nescafe, coca-cola), makanan yang unik
untuk individu (pulut, mee kuning, durian, buah pala) dll. Untuk mengelakkan
migraine, faktor penyebab perlulah dikenalpasti dan dielakkan".
MIGRAINE!
Migraine (from the Greek words hemi, meaning half, and
kranion, meaning skull) is a chronic neurological disorder characterized by
moderate to severe headaches, and nausea. It is about three times more common
in women than in men.
The typical migraine headache is unilateral (affecting one
half of the head) and pulsating in nature and lasting from four to 72 hours;
symptoms include nausea, vomiting, photophobia (increased sensitivity to light)
and phonophobia (increased sensitivity to sound); the symptoms are generally
aggravated by routine activity.
Approximately one-third of people who suffer from migraine headaches
perceive an aura—transient visual, sensory, language, or motor disturbances signalling
the migraine will soon occur.
Initial treatment is with analgesics for the headache, an
antiemetic for the nausea, and the avoidance of triggers. The cause of migraine
headache is unknown; the most supported theory is that it is related to
hyperexcitability of the cerebral cortex and/or abnormal control of painneurons
in the trigeminal nucleus of the brainstem.
Studies of twins indicate a 60- to 65-percent genetic
influence upon their propensity to develop migraine headaches. Moreover,
fluctuating hormone levels indicate a migraine relation: 75 percent of adult
patients are women, although migraine affects approximately equal numbers of
prepubescent boys and girls. Propensity to migraine headache sometimes
disappears during pregnancy, but in some women, migraines may become more
frequent.
Classification
The International Headache Society (IHS) offers guidelines
for the classification and diagnosis of migraine headaches, in a document
called "The International Classification of Headache Disorders, 2nd
edition" (ICHD-2). These
guidelines constitute arbitrary definitions, and are not supported by
scientific data.
According to ICHD-2, there are seven subclasses of
migraines (some of which include further subdivisions):
Migraine without aura, or common migraine, involves
migraine headaches that are not accompanied by an aura (visual disturbance, see
below).
Migraine with aura usually involves migraine headaches
accompanied by an aura. Less commonly, an aura can occur without a headache, or
with a non migraine headache. Two other varieties are familial hemiplegic
migraine and sporadic hemiplegic migraine, in which a patient has migraines
with aura and with accompanying motor weakness. If a close relative has had the
same condition, it is called "familial", otherwise it is called
"sporadic". Another variety is basilar-type migraine, where a
headache and aura are accompanied by difficulty speaking, vertigo, ringing in
ears, or a number of other brainstem-related symptoms, but not motor weakness.
Childhood periodic syndromes that are commonly precursors
of migraine include cyclical vomiting (occasional intense periods of vomiting),
abdominal migraine (abdominal pain, usually accompanied by nausea), and benign
paroxysmal vertigo of childhood (occasional attacks of vertigo).
Retinal migraine involves migraine headaches accompanied by
visual disturbances or even temporary blindness in one eye.
Complications of migraine describe migraine headaches
and/or auras that are unusually long or unusually frequent, or associated with
a seizure or brain lesion.
Probable migraine describes conditions that have some
characteristics of migraines, but where there is not enough evidence to
diagnose it as a migraine with certainty (in the presence of concurrent
medication overuse).
Chronic migraine, according to the American Headache
Society and the international headache society,
is a "complication of migraine"s and is a headache fulfilling
the diagnostic criteria for "migraine headache", which occurs for a
greater time interval. Specifically, greater or equal to 15 days/month for
greater than 3 months.
Signs and symptoms
Migraines typically present with recurrent severe headache
associated with autonomic symptoms. An
aura only occurs in a small percentage of people. The severity of the pain, duration of the
headache, and frequency of attacks is variable. A migraine lasting 72 hours is termed status
migrainosus and can be treated with
intravenous prochlorperazine. The four possible phases to a migraine
attack are listed below — not all the phases
are necessarily experienced. Additionally, the phases experienced and the
symptoms experienced during them can vary from one migraine attack to another
in the same person:
(1) The prodrome, which occurs hours or days before the
headache
(2) The aura, which immediately precedes the headache
(3) The pain phase, also known as headache phase
(3) The postdrome, the effects after the pain ended
Prodrome
Prodromal symptoms occur in 40–60% of those with migraines.
This phase may consist of altered mood, irritability, depression or euphoria,
fatigue, yawning, excessive sleepiness, craving for certain food (e.g.
chocolate), stiff muscles (especially in the neck), dizziness, hot ears,
constipation or diarrhea, increased or decreased urination, and other visceral
symptoms. These symptoms usually
precede the headache phase of the migraine attack by several hours or days, and
experience teaches the patient or observant family how to detect a migraine
attack is near.
Aura
For the 20–30% of
migraine sufferers who experience migraine with aura, this aura comprises focal
neurological phenomena that precede or accompany the attack. They appear
gradually over five to 20 minutes and generally last fewer than 60 minutes. The
headache phase of the migraine attack usually begins within 60 minutes of the
end of the aura phase, but it is sometimes delayed up to several hours, and it
can be missing entirely (see silent migraine). The pain may also begin before
the aura has completely subsided. Symptoms of migraine aura can be sensory or
motor in nature.
Visual aura is the
most common of the neurological events, and can occur without any headache.
There is a disturbance of vision consisting often of unformed flashes of white
and/or black or rarely of multicolored lights (photopsia) or formations of
dazzling zigzag lines (scintillating scotoma, often arranged like the
battlements of a castle, hence the alternative terms "fortification
spectra" or "teichopsia". Some patients complain of blurred or
shimmering or cloudy vision, as though they were looking at an area above a
heated surface, looking through thick or smoked glass, or, in some cases,
tunnel vision and hemianopsia.
The somatosensory aura of migraine may consist of
digitolingual or cheiro-oral paresthesias, a feeling of pins-and-needles
experienced in the hand and arm, as well as in the nose-mouth area on the same
side. The paresthesia may migrate up the arm and then extend to involve the
face, lips and tongue.
Other symptoms of the aura phase can include auditory,
gustatory or olfactory hallucinations, temporary dysphasia, vertigo, tingling
or numbness of the face and extremities, and hypersensitivity to touch.
Oliver Sacks's book Migraine describes "migrainous
deliria" as a result of such intense migraine aura that it is
indistinguishable from "free-wheeling states of hallucinosis, illusion, or
dreaming."
Pain
The typical migraine headache is unilateral, throbbing, and
moderate to severe, and can be aggravated by physical activity. Not all these features are necessary. The
pain may be bilateral at the onset or start on one side and become generalized,
and may occur primarily on one side or alternate sides from one attack to the
next. The onset is usually gradual. The pain peaks and then subsides and
usually lasts four to 72 hours in adults and one to 48 hours in children. The
frequency of attacks is extremely variable, from a few in a lifetime to several
a week, and the average sufferer experiences one to three headaches a month.
The head pain varies greatly in intensity, and can be very severe.
The pain of migraine is invariably accompanied by other
features. Nausea occurs in almost 90 percent of patients, and vomiting occurs
in about one third of patients. Many patients experience sensory
hyperexcitability manifested by photophobia, phonophobia, and osmophobia and
seek a dark and quiet room. Blurred vision, delirium, nasal stuffiness,
diarrhea, tinnitus, polyuria, pallor, or sweating may be noted during the
headache phase. There may be localized edema of the scalp or face, scalp
tenderness, prominence of a vein or artery in the temple, or stiffness and
tenderness of the neck. Impairment of concentration and mood are common. The
extremities tend to feel cold and moist.Vertigo
may be experienced; a variation of the typical migraine, called
vestibular migraine, has also been described. Lightheadedness, rather than true
vertigo, and a feeling of faintness may
occur.
Postdrome
The effects of migraine may persist for some days after the
main headache has ended. Many sufferers report a sore feeling in the area where
the migraine was, and some report impaired thinking for a few days after the
headache has passed. The patient may feel tired or "hungover" and
have head pain, cognitive difficulties, gastrointestinal symptoms, mood
changes, and weakness. According to one summary, "Some people feel unusually
refreshed or euphoric after an attack, whereas others note depression and
malaise.”
Cause
The underlying cause of migraines is unknown. There are, however, many biological events
that have been clinically associated with migraine.
Triggers. Migraines
may be induced by triggers, with some reporting it as an influence in a
minority of cases and others the majority.
Many things have been labeled as triggers, however the strength and
significance of these relationships are uncertain. Common triggers quoted are stress, hunger, and
fatigue (these equally contribute to tension headaches). A 2003 review concluded there was no
scientific evidence for an effect of tyramine on migraine. A 2005 literature review on dietary triggers
found the available scientific studies, mostly relying on subjective
assessments, were not rigorous enough to prove or disprove any particular
triggers. This is in line with other reviews. A 2009 review of potential
triggers in the indoor and outdoor environment concluded the overall evidence
was of poor quality, but nevertheless suggested migraineurs take some
preventative measures related to indoor air quality and lighting.
While monosodium glutamate (MSG) is frequently reported as
a dietary trigger evidence does not
consistently support this. Migraines
are more likely to occur around menstruation. Other hormonal influences, such
as menarche, oral contraceptive use, pregnancy, perimenopause, and menopause,
also play a role.
Depolarization. The phenomenon known as cortical spreading
depression, which is associated with the aura of migraine has been theorized as a possible cause of
migraines. In cortical spreading depression, neurological activity is initially
activated, then depressed over an area of the cerebral cortex. This situation
has been suggested to result in the release of inflammatory mediators leading
to irritation of cranial nerve roots, most particularly the trigeminal nerve,
which conveys the sensory information for the face and much of the head. This
theory is, however, speculative, without any supporting evidence, and there are
indeed cogent arguments against it. First, only about one third of migraineurs
experience an aura, and those who do not experience aura do not have cortical
spreading depression. Second, many
migraineurs have a prodrome, which occurs up to three days before the aura.
Vascular. Studies have shown the aura coincides with
constriction of blood vessels in the brain. This may start in the occipital
lobe, in the back of the brain, as arteries spasm. The reduced flow of blood
from the occipital lobe triggers the aura some individuals who have migraines
experience, because the visual cortex is in the occipital area.
When the constriction of blood vessels in the brain stops
and the aura subsides, the blood vessels of the scalp dilate. The walls of these blood vessels become
permeable and some fluid leaks out. This leakage is recognized by pain
receptors in the blood vessels of surrounding tissue. In response, the body
supplies the area with chemicals which cause inflammation. With each heart
beat, blood passes through this sensitive area, causing a throb of pain.
Although cerebral vasodilation can trigger migraine
attacks, blood vessel diameters return to normal more than an hour before the
migraine headaches occur.
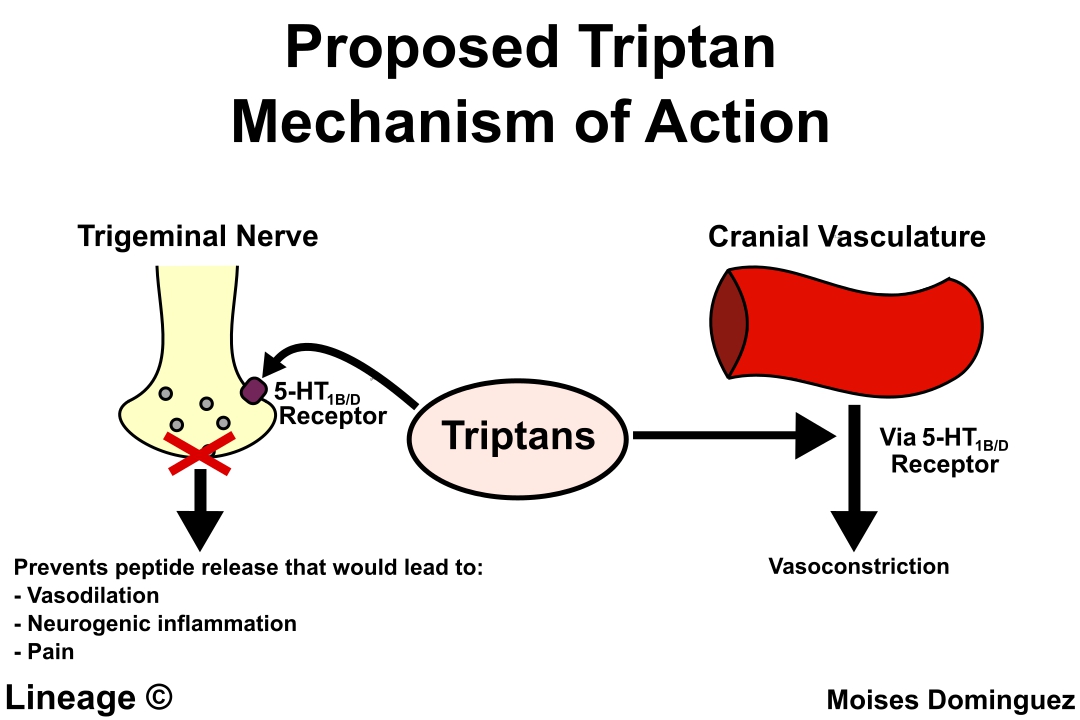
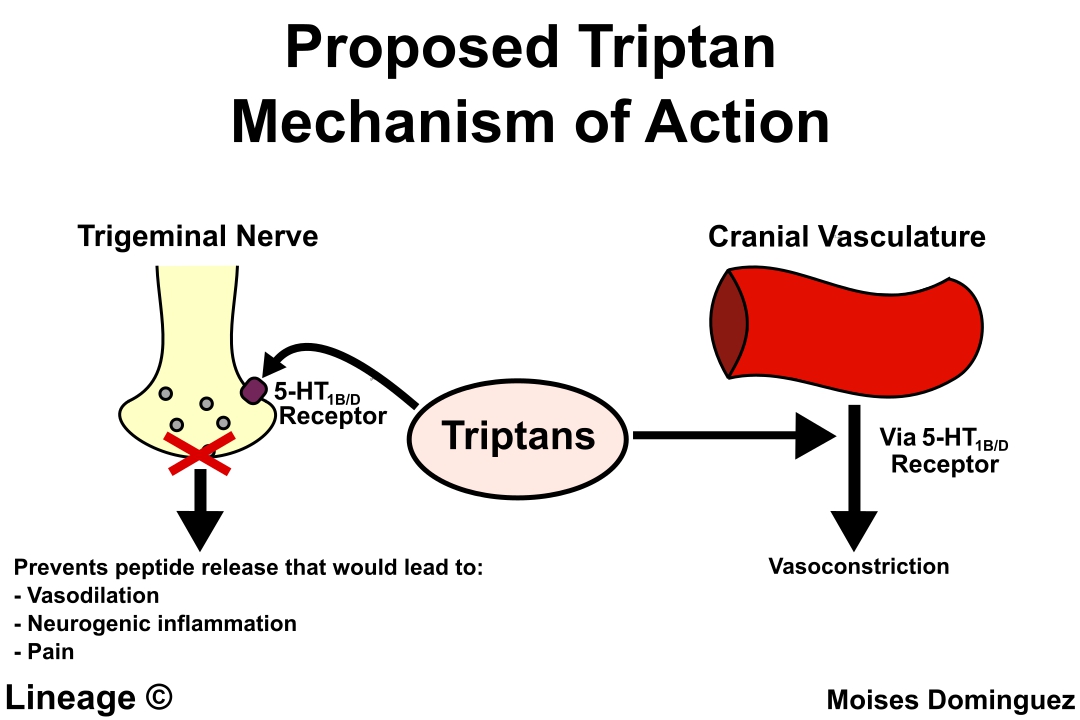
Serotonin. Serotonin
is a type of neurotransmitter, or "communication chemical" which
passes messages between nerve cells. It helps to control mood, pain sensation,
sexual behaviour and sleep, as well as dilation and constriction of the blood
vessels, among other things. Low serotonin
levels in the brain may lead to a process of constriction and dilation
of the blood vessels which trigger a migraine.
Serotonergic agonists, such as triptans, LSD or psilocin, activate
serotonin receptors to stop a migraine attack.
Melanopsin Receptor.
A melanopsin-based receptor has been linked to the association between
light sensitivity and migraine pain,
but this is currently speculation.
Neural. When certain
nerves or an area in the brain stem become irritated, a migraine begins. In
response to the irritation, the body releases chemicals which cause
inflammation of the blood vessels. These chemicals cause further irritation of
the nerves and blood vessels and results in pain. Substance P is one of the
substances released with first irritation. Pain then increases because
substance P aids in sending pain signals to the brain.
Unifying theory
Both vascular and neural influences cause migraines.
stress triggers changes in the brain
these changes cause serotonin and/or histamine to be
released
blood vessels constrict and dilate
chemicals, including substance P, irritate nerves and blood
vessels, causing neurogenic inflammation and pain.
Pathophysiology.
Migraine is a neurovascular disorder.
Although migraine is thought by some to be a neurological disease, in
the absence of scientific evidence, this remains a hypothesis.
Initiation
Migraines were once thought to be initiated exclusively by
problems with blood vessels, but the vascular changes of migraines are now
considered by some to be secondary to brain dysfunction, although this concept has not been supported
by the evidence. This was eloquently summed up by Dodick, who wrote,
"There is no disputing the role of the central nervous system in the
susceptibility, modulation and expression of migraine headache and the
associated affective, cognitive, sensory, and neurological symptoms and signs.
However, to presume that migraine is always generated from within the central
nervous system, based on the available evidence, is naïve at best and
unscientific at worst.The emerging evidence would suggest that just as
alterations in neuronal activity can lead to downstream effects on the cerebral
blood vessel, so too can changes within endothelial cells or vascular smooth
muscle lead to downstream alterations in neuronal activity. Therefore, there
are likely patients, and/or at least attacks in certain patients, where
primarily vascular mechanisms predominate.
Some have even attempted to show that vascular changes are of no
importance in migraine, but this claim
is unsubstantiated and has not been supported by scientific evidence. 'If we
swing between vascular and neurogenic views of migraine, it is probably because
both vascular and neurogenic mechanisms for migraine exist and are important'-
J Edmeads.
Pain
Although the initiating factor of migraine remains unknown,
copious, irrefutable evidence shows the pain of migraine (the third phase) is,
in some patients, related to painful dilatation of the terminal branches of the
external carotid artery, and in particular its superficial temporal and
occipital branches. Dilatation of the
arteries in the brain and dura mater previously was thought to be the origin of
the vascular pain, but these vessels have been shown to not dilate during
migraine. Because these arteries are
relatively superficial, it is easy to diagnose whether they are the source of
the pain. If they are, then they are also accessible to a form of migraine
surgery being promoted, largely to the efforts of Dr Elliot Shevel, a South
African surgeon, who has reported excellent success using the procedure.
Pericranial (jaw and neck) muscle tenderness is a common
finding in migraine. Muscle tenderness
has been shown to be present in 100% of migraine attacks, making muscle
tenderness the single most common finding in migraine. Tender muscle trigger points can be at least
part of the cause, and perpetuate most kinds of headaches.
Diagnosis
Migraines are underdiagnosed, and often are misdiagnosed. The diagnosis of migraine without aura,
according to the International Headache Society, can be made according to the
following criteria, the "5, 4, 3, 2, 1 criteria".
5 or more attacks - for migraine with aura, two attacks are
sufficient for diagnosis.
4 hours to 3 days in duration
2 or more of the following:
Unilateral (affecting half the head);
Pulsating;
"Moderate or severe pain intensity";
"Aggravation by or causing avoidance of routine
physical activity"
1 or more of the following:
"Nausea and/or vomiting";
Sensitivity to both light (photophobia) and sound
(phonophobia)
The mnemonic POUNDing (Pulsating, duration of 4–72 hOurs,
Unilateral, Nausea, Disabling) can help diagnose migraine. If four of the five
criteria are met, then the positive likelihood ratio for diagnosing migraine is
24. The presence of either disability, nausea or sensitivity can diagnose
migraine with:
(1) sensitivity of 81%
(2) specificity of 75%
Migraine should be differentiated from other causes of
headaches, such as cluster headaches. These are extremely painful, unilateral
headaches of a piercing quality. The duration of the common attack is 15
minutes to three hours. Onset of an attack is rapid, and most often without the
preliminary signs characteristic of a migraine.
Medical imaging of the head and neck may be used to rule
out secondary causes of headaches.
Prevention
Preventive (also called prophylactic) treatment of
migraines can be an important component of migraine management. Such treatments
can take many forms, including taking preventive drugs, migraine surgery,
taking nutritional supplements, lifestyle alterations, such as increased
exercise, and avoidance of migraine triggers.
The goals of preventive therapy are to reduce the
frequency, painfulness, and/or duration of migraines, and to increase the
effectiveness of abortive therapy.
Another reason to pursue these goals is to avoid medication overuse
headache (MOH), otherwise known as rebound headache. This is a common problem
among migraineurs, and can result in chronic daily headache.
Many of the preventive treatments are quite effective. Even
with a placebo, one-quarter of patients find their migraine frequency is
reduced by half or more, and actual treatments often far exceed this figure.
Medication
Before reading the medication process recommended by modern
medicine, let us see what is the medication efforts from the islamic
perspective.
Rawatan migraine dari perpektif perubatan islam:
Rujukan ini diambil dari Darussyifa' (oleh itu untuk mengamalkan perubatan kaedah
ini perlu merujuk terlebih dahulu kepada Darussyifa'.
Migraine ialah satu keadaan di mana sakit kepala terjadi
disebabkan oleh aliran darah dan perubahan kimia diotak. Perubahan ini akan
menyebabkan arteri yang membekalkan darah ke otak tersekat dan menimbulkan
sakit kepala yang diikuti oleh rasa tidak selesa pada perut, loya dan pening.
Ia juga kadangkala menimbulkan kesan kepada pandangan.
Migraine juga ialah sejenis penyakit keturunan. Wanita
mempunyai kecenderungan mengidap migrain yg lebih tinggi daripada lelaki.
Biasanya pesakit mengalami gejala gangguan saraf seperti
gangguan kepada pandangan seperti titik buta dan melihat motif seperti zig zag
sebelum mengalami sakit kepala;
Kadang-kadang pesakit melihat sinar cahaya yang amat terang
hingga tersa seperti hampir buta;
Selalunya gejala (1) dan (2) akan berlaku selama 15 hingga
20 minit dan diikuti dengan sakit kepala yang amat sangat. Pesakit akan biasa
mengalami sakit kepala yang teruk dan berdenyut denyut disebelah atau satu
bahagia kepala sahaja;
Ini akan diikuti oleh muntah atau cirit-birit.
SENARAI BACAAN AYAT-AYAT PENAWAR UNTUK PENYAKIT MIGRAINE:
Amalan Minggu Pertama dan Kedua:
1. Surah Al-Qasas ayat 51 hingga 59, baca 3 kali selepas
solat Magrib atau Isyak dan mohon doa kepada Allah s.w.t.
2. Surah Muhammad ayat 21 hingga 32, baca 3 kali selapas
solat Subuh atau waktu pagi dan mohon doa kepada Allah s.w.t.
Amalan minggu ketiga dan keempat:
1. Surah Asy-Syura ayat 17 hingga 26, baca 3 kali selepas
solat Maghrib atau Isyak dan mohon doa kepada Allah s.w.t.
2. Surah An-Naml ayat 71 hingga 81, baca 3 kali selapas
solat Subuh atau waktu pagi dan mohon doa kepada Allah s.w.t.
Sekali lagi: sila rujuk kepada Darussyifa'.

Selawat Syifa'
Now we look the conventional medic of migraine treatments.
Preventive migraine drugs are considered effective if they reduce the frequency
or severity of migraine attacks by at least 50%. The major problem with migraine preventive
drugs, apart from their relative inefficacy, is that unpleasant side effects
are common. So, preventive medication is limited to patients with frequent or
severe headaches.
Many medicines are available to prevent or reduce
frequency, duration and severity of migraine attacks. They may also prevent
complications of migraine. Beta blockers, such as Propranolol, atenolol, and
metoprolol; calcium channel blockers, such as amlodipine, flunarizine and
verapamil; the anticonvulsants sodium valproate, divalproex, gabapentin and
topiramate; and tricyclic antidepressants are some of the commonly used drugs.
Tricyclic antidepressants have been found to be more
effective than SSRIs. Tricyclic antidepressants have been long established as
efficacious prophylactic treatments. These
drugs, however, may give rise to undesirable side effects, such as insomnia,
sedation or sexual dysfunction. There is no consistent evidence that SSRI antidepressants are effective for migraine
prophylaxis. While amitryptiline (Elavil) is the only tricyclic to have
received FDA approval for migraine treatment, other tricyclic antidepressants
are believed to act similarly and are widely prescribed, often to find one with
a profile of side effects that is acceptable to the patient.
In addition to tricyclics a, the antidepressant nefazodone
may also be beneficial in the prophylaxis of migraines due to its antagonistic
effects on the 5-HT2A and 5-HT2C receptors.
It has a more favorable side effect profile than amitriptyline, a
tricyclic antidepressant commonly used for migraine prophylaxis.
Antidepressants offer advantages for treating migraine patients with comorbid
depression. SSRIs are not approved by
theFDA for treatment of migraines, but have been found to be effective by some
practitioners.
There is some evidence that low-dose asprin has benefit for
reducing the occurrence of migraines in susceptible individuals.
Surgery
Migraine surgery is
a field that shows a great deal of promise, particularly in those who suffer
more frequent attacks, and in those who have not had an adequate response to
prophylactic medications. Patients often still experience a poor quality of
life despite an aggressive regimen of pharmacotherapy. For these reasons, surgical solutions to
migraines have been developed, which have excellent results.
A major advantage of
migraine surgery is that, with the correct diagnostic techniques, a definite
diagnosis can be made before the surgery is undertaken. Once a positive
diagnosis has been made, the results of surgery are outstanding and provide
permanent pain relief, as well as relief from the associated symptoms, such as
nausea, vomiting, light sensitivity, and sound sensitivity. Surgical
cauterization of the superficial blood vessels of the scalp (the terminal
branches of the external carotid artery) is only carried out if it has been
established with certainty that these vessels are indeed the source of pain. It
is a safe and relatively atraumatic procedure which can be performed in a day
facility. The value of arterial sugery
for migraine treatment is gaining recognition as a result of the efforts of a
South African surgeon, Dr Elliot Shevel, who has produced a number of papers on
the subject.
The removal of muscles or nerves in areas known as
"trigger sites" provides good results, but only in patients who
respond well to Botox injections in specific areas. There is also evidence that the correction of
a congenital heart defect, patent foramen ovale (PFO), reduces migraine
frequency and severity. Recent studies
have advised caution, though, in relation to PFO closure for migraines, as insufficient
evidence exists to justify this dangerous procedure.
Other therapies
Medical devices, such as biofeedback and neurostimulators,
have some advantages in the migraine treatment, mainly when common antimigraine
medication is contraindicated or in case of medication over use.
Biofeedback helps patient to be conscious
of some physiologic parameters to control them and try to relax. This method is
considered to be efficient for migraine and tension-type headache
treatment. A recent clinical trial has
demonstrated that simple use of biofeedback as a relaxation technique has
similar efficacy for migraine treatment to sophisticated sessions in clinics.
Neurostimulation used initially implantable
neurostimulators similar to pacemakers for the treatment of intractable chronic
migraines with encouraging good results.
But the needed surgery with implantable neurostimulators is limiting the
indication to sever cases. Recently, a
new technique of external trigeminal (V1) or occipital nerve (CII)
neurostimulation (Cefaly) could offer a larger use for migraine treatment or
prevention.
A systematic review stated that chiropractic manipulation,
physiotherapy, massage and relaxation might be as effective as propranolol
ortopiramate in the prevention of migraine headaches; however, the research had
some problems with methodology.
"The therapeutic potential of magnesium, coenzyme
Q(10), riboflavin, and vitamin B(12) can be cautiously inferred from some
published open clinical trials. A review
has concluded that "current clinical data support the use of fever-few,
butterbur, magnesium, and riboflavin in migraine prophylaxis."
Migraine diary. A
migraine diary allows the assessment of headache characteristics, to
differentiate between migraine and tension-type headache and to record the use
and efficacy of acute medication. A diary also helps to analyse the
relationship between migraine and menstruation. Finally, the diary can help to
identify trigger factors. A trigger may occur up to 24 hours prior to the onset
of symptoms; the majority of migraines,
though, are not caused by identifiable triggers.
Management. There
are three main aspects of treatment: trigger avoidance, acute symptomatic
control, and pharmacological prevention. Medications are more effective if used
earlier in an attack. The frequent use of medications may, however, result in
medication overuse headache, in which the headaches become more severe and more
frequent. These may occur with triptans, ergotamines, and analgesics,
especially arcotic analgesics.

Analgesics
A number of analgesics are effective for treating migraines
including:
(1) Non-steroidal anti-inflammatory drugs (NSAIDs): Ibuprofen
provides effective pain relief in about half of people. Naproxen can abort about one third of
migraine attacks, which was 5% less than the benefit of sumatriptan. A 1000 mg
dose of aspirin could relieve moderate to severe migraine pain, with similar
effectiveness to sumatriptan.
(2) Paracetamol/acetaminophen, either alone or in combination
with metaclopramide, is effective for migraines.
Simple analgesics combined with caffeine may help. Even by itself, caffeine can be useful during
an attack, despite, in general, migraine
sufferers are advised to limit their caffeine intake.

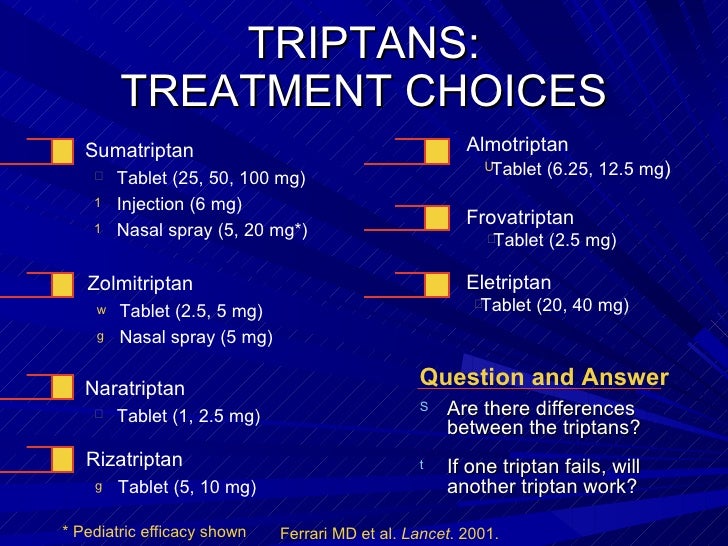
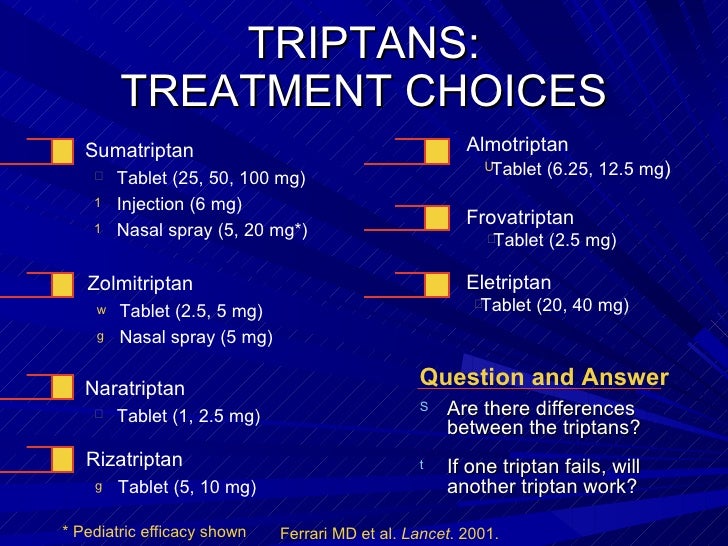
Triptans
Triptans such as sumatriptan are effective for both pain and nausea in up
to 75% of people. The different forms
available include oral, injection, nasal spray, and oral dissolving
tablets. Most side effects are mild,
such as flushing; however, rare cases of myocardial ischemia have
occurred. They are not addictive, but
may cause medication overuse headaches if used more than 10 days per month.
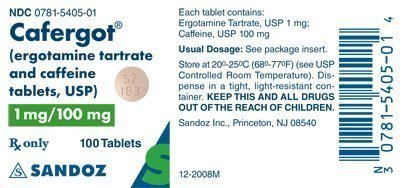
Ergotamines
Ergotamine and
dihydroergotamine are older medications
still prescribed for migraines, the latter in nasal spray and injectable
forms. They were the primary drugs
available to abort a migraine prior to the triptans, and are much less
expensive than triptans.
Corticosteroids
A single dose of intravenous dexamethasone, when added to
standard treatment of a migraine attack, is associated with a 26% decrease in
headache recurrence in the following 72 hours.

Other Symptoms
Antiemetics by mouth may help relieve symptoms of nausea
and help prevent vomiting, which can diminish the effectiveness of orally taken
analgesics. In addition, some antiemetics, such as metoclopramide, are
prokinetics and help gastric emptying,
which is often impaired during episodes of migraine. In the UK, three
combination antiemetic and analgesic preparations are available: MigraMax
(aspirin with metoclopramide), (paracetamol/codeine for analgesia, with
buclizine as the antiemetic) and
paracetamol/ metoclopramide (Paramax in UK). The earlier these drugs are taken in the
attack, the better their effect.
Prognosis
The risk of stroke may be increased two- to three-fold in
migraine sufferers. Young adult sufferers and women using hormonal contraception
appear to be at particular risk. The mechanism of any association is unclear,
but chronic abnormalities of cerebral blood vessel tone may be involved. Women
who experience auras have been found to have twice the risk of strokes and
heart attacks over nonaura migraine sufferers and women who do not have
migraines. (Note: Women who experience
auras and also take oral contraceptives have an even higher risk of stroke).
Migraine sufferers seem to be at risk for both thrombotic and hemorrhagic
stroke as well as transient ischemic attacks.
Death from cardiovascular causes was higher in people with migraine with
aura in a Women's Health Initiative study, but more research is needed to
confirm this.
I always curious to know more about how we can enhance our skill, how we can improve our portfolio to add some attractive certificate. I got some valuable points through this blog. Hair Loss Treatment
ReplyDelete